If you’ve ever worried about the possible long-term effects of being on Testosterone, you can relax because science has your back.
Italian researchers have concluded that “Testosterone administration in FtM subjects has a good safety profile” after finding “no significant serious adverse effects and no clinically relevant changes” in 45 FTM patients treated for at least 10 years with Testosterone.
Also notable: “Liver and kidney function tests did not show any significant changes.”
The aim of the study was to assess the effects and safety of Testosterone administration on body weight, lipid profile, hematological and bone parameters in trans men.
Largest Study to Date: Transgender Hormone Treatment Safe
The largest study to date investigating the safety of cross-sex hormone treatment of transgender adults confirmed the findings of smaller studies performed over the past decade, concluding that treatment is safe and leads to very few long-term side effects.
More than 2000 patients from 15 US and European centers participated in the retrospective 2014 study. 523 were female to male (FTM) and had a follow-up of 4.5 years and age of 27.5 years. The FTM subjects most often had the following side effects: acne with local treatment (2.9%, n = 15), weight gain (0.4%; n = 2), muscle pain (0.4%; n = 2), and liver-enzyme abnormalities (0.4%; n = 2).
“Our results are very reassuring,” said principal investigator Henk Asscheman, MD, PhD. “There are mostly minor side effects and no new [adverse events] observed in this large population.”
Prior to this landmark study, several other studies had already indicated the a good safety profile for Testosterone therapy.
- The European Journal of Endocrinology published a paper in 2011 (Asscheman et al.) presenting mortality data from more than a thousand transsexuals followed for a median time of 18 years and who had undergone previous or were currently on long term cross-sex hormonal treatment. Researchers concluded that, “In the FtM transsexuals, use of testosterone in doses used for hypogonadal men seemed safe.”
- A 2010 study published in the Journal of Sexual Medicine relied on evidence derived from studies in female-to-male transsexuals treated with Testosterone for long periods of time with no apparent major adverse effects. No increase in mortality, breast cancer, vascular disease, or other major health problems were reported.
- The prominent Dutch endocrinologist Dr. Louis Gooren led a study in 2008 that reviewed data from the Amsterdam gender clinic from 1975 up to 2006, which included 876 female-to-male transsexuals who received cross-sex hormone treatment. He concluded that Testosterone is acceptably safe over the short and medium term, but referenced a lack of solid data and did not go as far to claim long-term safety.
- In the early 2000s, there were concerns about the increased cardiovascular risk with testosterone therapy in cisgender men, which resulted in an FDA warning. Recent studies found that these risks did not show an increase or improved cardio vascular outcomes in hypogonadal men who received testosterone therapy.
More recently in 2018, researchers analyzed outcomes from three different sites in the Kaiser Permanente health care system. Changes in lipid profiles in transmasculine patients included an increase in LDL and triglycerides and a decrease in HDL. This pattern is similar to what is seen in cisgender men receiving testosterone therapy. There is inconclusive evidence on the result of these lipid changes, particularly for increased or decreased cardiovascular risk. In this patient population, testosterone therapy did not result in a significant increase in short-term death, stroke, MI and thromboembolic disease.
A just-published review study also found that transgender men who have undergone hormone replacement therapy for over 10 years haven’t had any increase in cardiovascular disease.
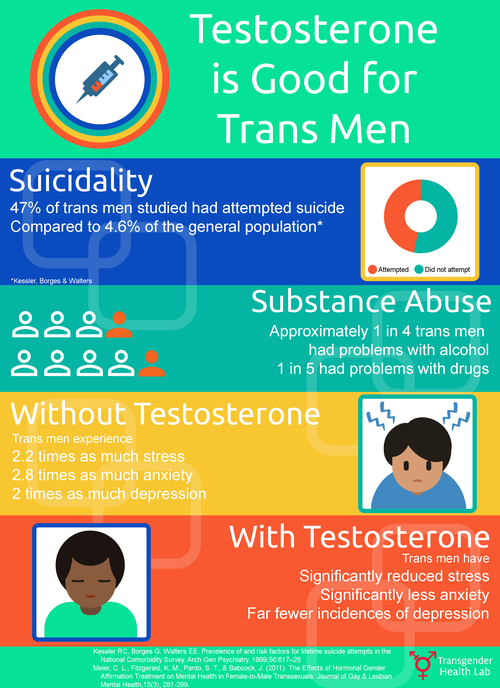
We also know that Testosterone is good for trans masculine folks!
In 2014, researchers reported that, “Results indicate that testosterone treatment in FTMs is associated with a positive effect on mental health on measures of depression, anxiety, and anger.” The following year, another study published findings that suggest that “testosterone treatment resulted in increased levels of psychological functioning on multiple domains in transgender men relative to nontransgender controls,” indicating “a direct positive effect of 3 months of testosterone treatment on psychological functioning in transgender men.”
Source: http://coltkeo-meier.com/research
Meier, C., Fitzgerald, K., Pardo, S., & Babcock, J. (2011). The effects of hormonal gender affirmation treatment on mental health in female-to-male transsexuals. Journal of Gay and Lesbian Mental Health, 15(3), 281-299.
References
Safety
of More Than Ten Years Testosterone Administration in FTM Subjects.
Cristina Meriggiola, MD, PhD, Antonietta Costantino, PhD,
Carla Pelusi, MD, Martina Lambertini, MD, Alberto Bazzocchi, MD. Book
of Abstracts, WPATH 2014 Biennial International Symposium
A long-term follow-up study of mortality in transsexuals receiving treatment with cross-sex hormones. – FULL TEXT
Asscheman H, Giltay EJ, Megens JA, de Ronde WP, van Trotsenburg MA, Gooren LJ. Eur J Endocrinol. 2011 Apr;164(4):635-42.
Safety of physiological testosterone therapy in women: lessons from female-to-male transsexuals(FMT) treated with pharmacological testosterone therapy.
Traish AM, Gooren LJ. J Sex Med. 2010 Nov;7(11):3758-64.
Long-term treatment of transsexuals with cross-sex hormones: extensive personal experience.
Gooren LJ, Giltay EJ, Bunck MC. J Clin Endocrinol Metab. 2008 Jan; 93(1):19-25. Epub 2007 Nov 6.
Effects of Testosterone Treatment and Chest Reconstruction Surgery on Mental Health and Sexuality in Female-To-Male Transgender People
Samuel A. Davis & S. Colton Meier (2014). International Journal of Sexual Health, 26:2, 113-128.
Testosterone treatment and MMPI-2 improvement in transgender men: a prospective controlled study.
Keo-Meier CL, Herman LI, Reisner SL, Pardo ST, Sharp C, Babcock JC. J Consult Clin Psychol. 2015 Feb;83(1):143-56. Epub 2014 Aug 11.

